Cancer is a complex disease with patients becoming at high risk of malnutrition both as a consequence of their illness and its treatment1. Over 50% of cancer patients present with weight loss at diagnosis and, for many patients, nutritional status continues to deteriorate during and after treatment.2,3

Up to 80% of all cancer patients will be malnourished.4
Cancer related malnutrition is driven by a combined effect of reduced nutritional intake and metabolic changes5-7. These factors contribute to negative energy and protein balance leading to weight and muscle mass loss1.
Poor nutritional status in addition to weight and muscle mass loss can lead to poorer outcomes for the patient. Clinically this impacts not only the patient but also the healthcare setting in a number of ways.
Patient impact
- Lower quality of life8
- Increased risk of treatment interruption or delay9
- Decreased survival9-11
- Decreased physical function12
Healthcare setting impact
- Extended hospital stays13,14
- Increased risk of hospital re-admissions13,14
- Increased costs of hospitalisation13,14
- Increased post surgery complications15
Importance of good nutrition in cancer patients
Managing Malnutrition in Oncology
Identification of Malnutrition
Identification of malnutrition through screening is imperative, as recognised by the National Institute for Health and Care Excellence (NICE)16 and the European Society for Clinical Nutrition and Metabolism (ESPEN).5,17 Screening should be performed at the time of diagnosis.
Early nutritional intervention is key to support patient outcomes
Benefit of nutritional intervention on several quality of life aspects during treatment.18
Up to 50% reduction in post-operative complications after pre-operative ONS intervention.19,20
Up to a 3-day reduction in length of hospital stay.20
20% increase in probability of survival following early nutritional intervention and weight gain in some cancer patients.21

Oral Nutritional Supplements can play a role in a Cancer Patients Journey
ESPEN (2016)5 and ESPEN (2021)17 highlight the role that nutritional intevention plays in Oncology patients
“Nutritional interventions are recommended to increase oral intake in cancer patients who are able to eat but are malnourished or at risk of malnutrition. This includes dietary advice, the treatment of symptoms and derangements impairing food intake (nutrition impact symptoms), and offering oral nutritional supplements.”
Oral nutritional supplements in Oncology
The causes of reduced nutritional intake are complex and multifactorial.5 Two prevelant causes of malnutrition in oncology patients are taste disturbance and poor appetite:
Taste and smell alterations may develop throughout the course of the disease, before, during and up to one year after treatment.5 Taste alterations could lead to a reduced intake of food and therefore have a negative impact on the nutritional status with up to 25% reduction in nutritional intake, leading to greater weight loss.22,23
Fortisip Compact Protein - innovative taste sensations
The Fortisip Compact Protein range has been developed with a wide range of flavours, providing a flavour variety to your patients can help prevent taste fatigue.24 A high energy, high protein, low volume ONS with specific warming and cooling sensations appreciated in patients with Cancer.* Addressing the needs of taste alterations in cancer through creating sensations could help with compliance.

Low volume ONS may make it easier to consume the energy levels needed25, 26, particularly with reported side effects in oncology patients. Compliance with low volume 125ml ONS is significantly better than standard ONS.25,26
Compliance with ONS
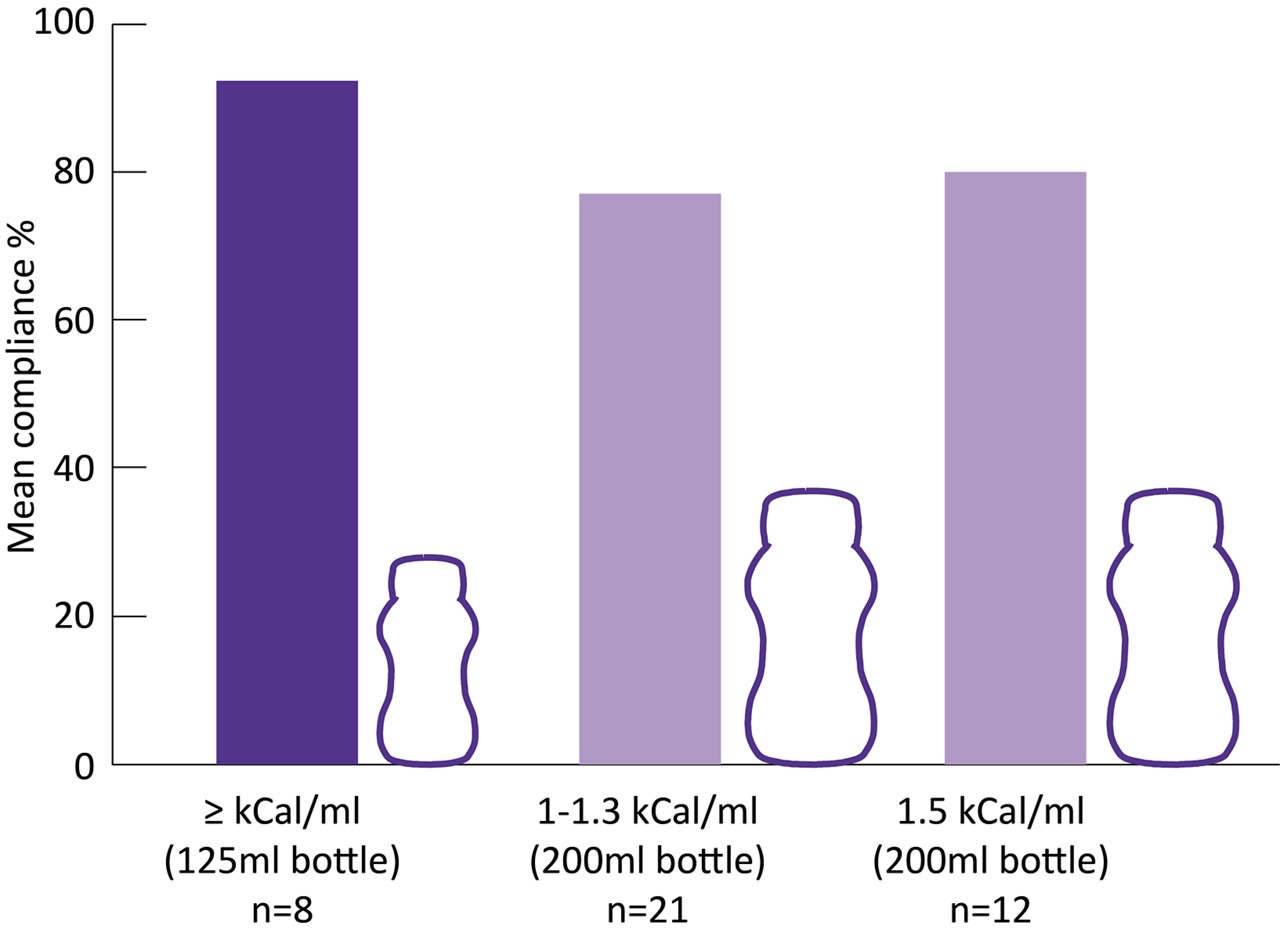
Adapted from Hubbard et al. 201226
Fortisip Compact Protein - high energy, high protein, low volume
Fortisip Compact Protein has been developed, offering a high energy, high protein, low volume ONS with 90% compliance.27
Do you have a question?
Contact our team of experts for guidance on the use and composition of our product range, for support with queries regarding your Nutricia account and sampling service or to get in touch with your local Nutricia representative. We are available Monday to Thursday 9am-5pm and Friday 9am-4pm (except Bank Holidays)

- Arends, et al. Clin Nutr. 2017;36(5):1187-1196.
- DeWys WD et al. 1980; 69: 491-497.
- Stratton RJ et al. 2003.
- Ravosco, et al. J Clin Med. 2019; 8:1211.
- Arends et al. Clin Nutr. 2016;36(1):11-48
- Marín Caro et al. Clin Nutr. 2007;26(3):289-301
- Fearon, et al. Lancet Oncol. 2011;12(5):489-495.
- Sánchez-Lara, al. Nutr Cancer. 2012;64(4):526-534
- Ross et al. Br J Cancer. 2004;90(10):1905-1911.
- Martin et al. J Clin Oncol. 2015;33(1):90-99.
- Gannavarapu et al. J Oncol Pract. 2018;14(4):e238-e250
- Mariani et al. Support Care Cancer. 2012;20(2):301-309
- Planas et al. Support Care Cancer. 2016;24(1):429-435.
- Gourin et al. Ann Otol Rhinol Laryngol. 2014;123(2):101-110.
- Yu et al. Eur J Clin Nutr. 2013;67(7):732-737
- NICE. Nutrition support for adults: oral nutrition support, enteral tube feeding and parenteral nutrition. Clinical Guideline CG32. https://www.nice.org.uk/Guidance/CG32 [Accessed October 2020].
- Muscaritoli, Arends, Bachmann et al. Clin Nutr. 2021; 40: 2898-2913
- Baldwin et al. J Natl Cancer Inst. 2012, 104(5): 371-385
- Kabata et al. Support Care Cancer. 2015; 23: 365-370.
- Maňásek et al. Klin Onkol. 2016; 29: 351-357.
- Trestini et al. Eur J Clin Nutr. 2018;72:772-779
- Spotten et al. Ann Oncol. 2017;28(5):969-984.
- Brisbois et al. J Pain Symptom Manage. 2011;41(4):673-683.
- Ravasco. Eur J Oncol Nurs. 2005;9 Suppl 2:S84-91.
- Hubbard et al. Prov Nutr Soc. 2010;69E164
- Hubbard GP et al. Clin Nutr. 2012;31(3):293-312.
- Brown et al. Journal of Nutrition, Health and Ageing. 2020;24:305–11.
- Cawood et al. Ageing Res. Rev 2012;11(2):278-96
*de Haan et al. Support Care Cancer. 2021. . https://doi.org/10.1007/s00520-021-06049-4



