Cow’s Milk Allergy, also known as Cow’s Milk Protein Allergy or CMPA, is one of the most common childhood allergies, affecting an estimated 2-5% of infants under the age of one1-3.
Whilst most infants grow out of a Cow’s Milk Allergy as they get older, managing the symptoms day-to-day can be difficult, not to mention distressing for parents and carers to deal with. To help with this, an early and accurate diagnosis is important, especially when it comes to identifying the appropriate management and reducing the need for elimination diets4.
In this article, we’ll be covering the main symptoms of a Cow’s Milk Allergy, the differences between a milk allergy and lactose intolerance, and how long it should take for any symptoms to settle down.
What is Cow’s Milk Allergy (CMA)?
A Cow’s Milk Allergy occurs when the immune cells in the body react abnormally to the proteins found in cow’s milk5.
There are two main types of Cow’s Milk Allergy, and we’ll be discussing the differences between them further along in the article. The two types are1-3,5 :
- Immediate Cow’s Milk Allergy or IgE mediated Cow’s Milk Allergy, and
- Delayed or non-IgE mediated Cow’s Milk Allergy.
In most cases, a Cow’s Milk Allergy will start during the first year of life5,8. Around 20% of infants will grow out of their Cow’s Milk Allergy by their first birthday, and most will no longer display CMA symptoms by the age of three7.
Cow’s Milk Allergy symptoms in infants
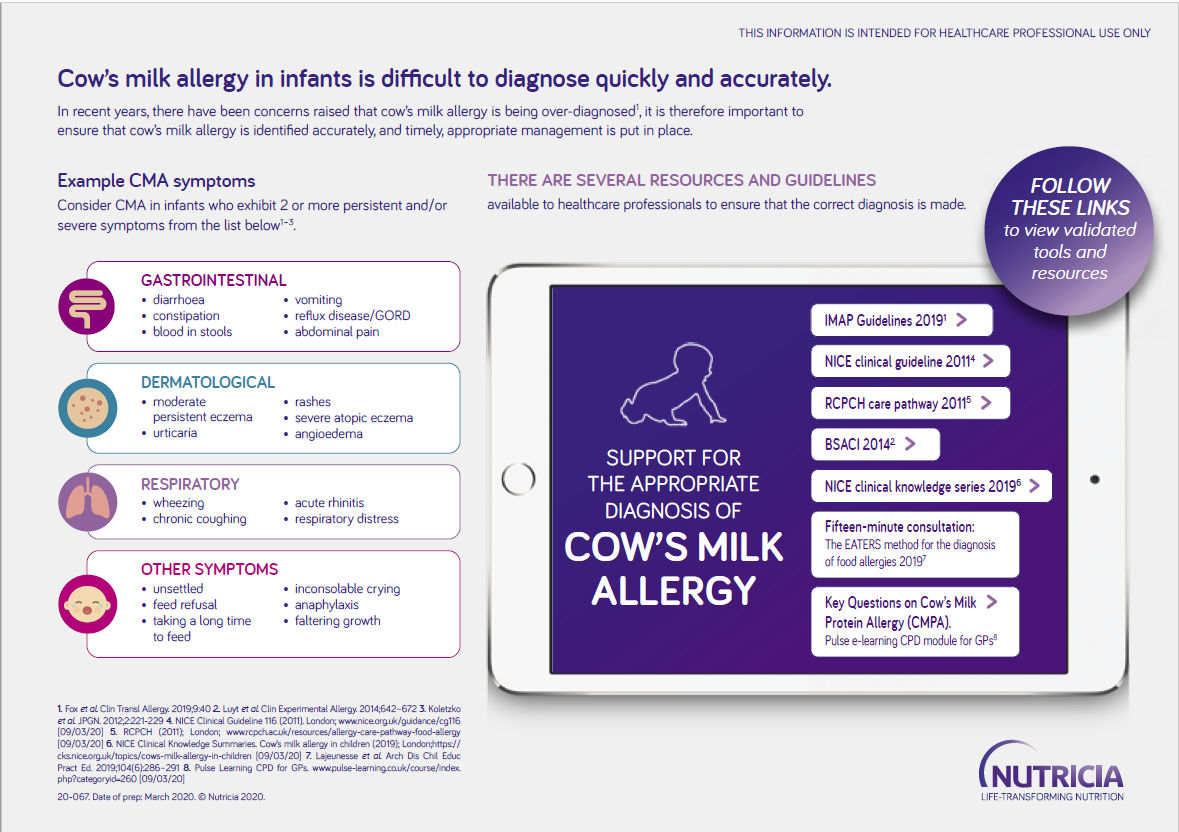
Cow’s Milk Allergy symptoms in infants can be numerous and can vary from case to case. Symptoms can be gastrointestinal, dermatological, or respiratory and include1-5:
- Skin reactions such as angioedema and atopic eczema
- Gastro-oesophageal reflux disease
- Digestive problems like abdominal pain, vomiting, diarrhoea or constipation
- Wheezing and chronic coughing
- Other symptoms such as inconsolable crying or persistent feed refusal are also possible, but care should be taken when interpreting these non-specific symptoms and not taken in isolation
Whilst very rare, a Cow’s Milk Allergy can cause anaphylaxis, a severe allergic reaction that requires immediate medical attention. The symptoms of anaphylaxis include swelling of the mouth or throat, coughing, wheezing and breathing difficulties8.
Signs of Cow’s Milk Allergy in a breastfed infant
Cow’s Milk Allergy symptoms usually start once cow’s milk is introduced into an infant’s diet. This can either be through formula milk, or when they begin weaning and eating solid foods6.
However, Cow’s Milk Allergy can also affect infants who are exclusively breastfed, albeit much less frequently so4. This is because the allergy-causing proteins can be transferred to infants via breast milk6,8, causing an allergic reaction.
Signs of milk allergy in a breastfed infant are generally the same as outlined above, but the method of management is likely to differ. Where breastfed infants present with CMA symptoms, the mother may be advised to follow a cow’s milk protein-free diet to see if this makes a difference1-3.
For more information on breastfeeding infants with cow's milk allergy, visit the article Breastfeeding and Cow's Milk Allergy.
Cow’s Milk Allergy vs lactose intolerance symptoms
When it comes to milk allergy vs lactose intolerance symptoms, there are a number of similarities. However, a Cow’s Milk Allergy is not the same as lactose intolerance.
Understanding the difference is vital when it comes to getting a swift, and correct, diagnosis, so that an effective dietary management plan can be put in place. You can read more about the differences between the two here.
IgE vs non-IgE milk allergy symptoms
A Cow’s Milk Allergy can be either immediate IgE (immunoglobulin E) or delayed non-IgE mediated. With an IgE milk allergy, the symptoms are immediate and will often appear within minutes of consuming cow’s milk protein. Non-IgE milk allergy symptoms, however, tend to develop anywhere from several hours to a few days after the consumption of cow’s milk protein1-3,6,8.
A non-IgE Cow’s Milk Allergy is often accompanied by a range of symptoms, including treatment-resistant atopic eczema, but they can also include vomiting, abdominal pain, constipation or diarrhoea1-3. Around half of CMA cases seen in the UK may present with delayed reactions12, frequently with gastrointestinal symptoms, making it challenging to diagnose1.
The symptoms of an IgE allergy to milk range from mild reactions to severe anaphylaxis. This might begin as swelling around the lips and eyes, rashes, vomiting, and in serious cases could lead to breathing difficulties9.
IgE vs non-IgE milk allergy symptoms
Symptoms of a non-IgE mediated Cow’s Milk Allergy will often show up in the form of gastrointestinal problems, which, rather unhelpfully, can easily be confused with the signs of lactose intolerance1.
Cow's Milk Allergy gastrointestinal symptoms include, but aren’t limited to1-2,6:
- Constipation or diarrhoea
- Vomiting
- Abdominal discomfort
- Blood in the stools
Is constipation a sign of Cow’s Milk Allergy in infants?
Whilst constipation may well be a sign of a milk allergy, it can also be the result of dietary changes, dehydration or a lack of fibre10. It’s important to understand the cause of constipation before making any diagnosis based on this one symptom alone.
Rash and other dermatological Cow’s Milk Allergy symptoms
Rashes, itchiness and swelling around the eyes, face or mouth can also be signs of a Cow’s Milk Allergy1-4,9. Whilst milder rashes and itchiness might point towards a non-IgE Cow’s Milk Allergy, serious swelling is usually a sign of an IgE mediated allergy, which could lead to anaphylaxis.
Is eczema a sign of a Cow’s Milk Allergy?
Eczema isn’t necessarily symptomatic of a milk allergy in isolation. However, eczema can be a symptom of a food allergy, especially if resistant to treatment1-2,5. In cases where eczema is accompanied by other CMA symptoms, then the possibility of a cow’s milk allergy should be explored.
Congestion and other respiratory symptoms of CMA
A Cow’s Milk Allergy might also present with respiratory symptoms. For instance, congestion, as well as chronic coughing and wheezing. Although rare, in more serious cases, this could progress to respiratory distress and anaphylaxis.
How long does it take to experience relief from symptoms of Cow’s Milk Allergy?
After diagnosis and appropriate management, how long it will take for a Cow's Milk Allergy to resolve depends upon the severity of the symptoms. Whilst some will experience relief from symptoms immediately once cow’s milk protein has been removed from their diet, for others it will take longer11.
In cases where a Cow’s Milk Allergy is suspected, there’s a recommended time frame of between 2-4 weeks to see an improvement in symptoms. Whereas in cases where a Cow’s Milk Allergy is diagnosed, it’s recommended that cow’s milk is removed from the diet for at least 6 months, and until the infant is between 9-12 months old1-5.
Whilst there’s no definite time frame here, up to 90% of infants will outgrow their Cow’s Milk Allergy and stop experiencing CMA symptoms by the age of three7.
Those infants with an immediate IgE Cow’s Milk Allergy may take longer to outgrow the symptoms than those with a delayed non-IgE allergy, but every infant is different and the age at which a Cow’s Milk Allergy is outgrown can vary. It’s also dependent upon a number of factors, including how severe the CMA symptoms are, how old they were at the onset of the allergy and whether there are other allergies at play1,7.
- Luyt D, et al. BSACI guideline for the diagnosis and management of cow's milk allergy. Clin Exp Allergy. 2014;44(5):642-672. doi:10.1111/cea.12302.
- Fox A, et al. An update to the Milk Allergy in Primary Care guideline. Clin Transl Allergy. 2019; 12;9:40.
- Koletzko S, et al. Diagnostic approach and management of cow's-milk protein allergy in infants and children: ESPGHAN GI Committee practical guidelines. J Pediatr Gastroenterol Nutr. 2012;55(2):221-9
- Vandenplas Y, et al. Guidelines for the diagnosis and management of cow’s milk protein allergy in infants. Archives of Disease in Childhood 2007;92:902-908.
- NICE. Clinical Knowledge Summary. Cow’s milk Allergy in Children. [internet] [updated 2021 August; cited 2023 January 12]. Available from:https://cks.nice.org.uk/topics/cows-milk-allergy-in-children/#:~:text=Cow%27s%20milk%20allergy%20is%20a,more%20proteins%20in%20cow%27s%20mil
- NHS. What should I do if I think my baby is allergic or intolerant to cow’s milk? [internet] [updated 2022 November 28; cited 2023 January 12]. Available from: https://www.nhs.uk/common-health-questions/childrens-health/what-should-i-do-if-i-think-my-baby-is-allergic-or-intolerant-to-cows-milk/
- The GP Infant Feeding Network. Cow’s Milk Allergy. [internet] [updated 2019 October 8; cited 2023 January 12]. Available from: https://gpifn.org.uk/cma/#:~:text=In%20the%20case%20of%20non,improvement%20during%20the%20exclusion%20period [Accessed January 2023]
- Allergy UK. What is a cow’s milk allergy? [internet] [updated 2023; cited 2023 January 12]. Available at https://www.allergyuk.org/about-allergy/allergy-in-childhood/cows-milk-allergy/#download_access
- NHS. Food allergy. [internet] [updated 2023 January 5; cited 2023 January 12]. Available from: https://www.nhs.uk/conditions/food-allergy/
- NHS Start4Life. Breastfeeding challenges. [internet] [updated 2022; cited 2023 January 12]. Available from: https://www.nhs.uk/start4life/baby/feeding-your-baby/breastfeeding/breastfeeding-challenges/constipation/#:~:text=Treating%20constipation&text=If%20your%20baby%20is%20happy,are%20particularly%20good%20for%20constipation
- AllergyUK, 2023. Your baby’s cow’s milk allergy journey. [internet] [updated 2022; cited 2023 January 12]. Available from: https://www.allergyuk.org/resources/cma-roadmap/#:~:text=Whilst%20many%20babies%20may%20have,get%20support%20during%20this%20time
- Schoemaker A, et al. Incidence and natural history of challenge-proven cow's milk allergy in European children--EuroPrevall birth cohort. Allergy. 2015 ;70(8):963-72.
You may also be interested in
Help us provide information most relevant to you
Please ensure your role and areas of interest are up to date.