Martine’s Story
Behind every one of our nutritional solutions there is a dedicated team of people whose mission it is to make the lives of patients and healthcare professionals, easier. #NutriciaLife
Martine has been a Nutricia Homeward Nurse for 12 years. The Nutricia Homeward service supports more than 29,000 home tube fed patients every year. There are over 160 Nutricia Homeward nurses like Martine, each of whom is committed to providing the skills and reassurance to help patients manage home enteral feeding and to stay out of hospital.
I started my nursing career 33 years ago, initially working for the NHS, and then going to work in the private sector. The rewarding nature of the job, combined with stability and job variation motivated me to pursue a career in nursing. After 14 years I decided to see what else was out there and I stumbled across Nutricia, because I’d ended up working with some of the Nutricia Homeward nurses in Halifax and Huddersfield and I absolutely loved it. They were so professional, and just a lovely team to work with. I was blown away. I wanted to be one of them. That’s how it all started.
I was really struck by their independence and the support that they had from Nutricia, as well as the camaraderie between the nurses themselves. As a Nutricia Homeward nurse, you’re working autonomously and using your own diary, so you’ve got to be really organised. I’m part of the North West nursing team, covering the areas stretching from Cumbria to Halifax and Huddersfield, all the way down to Manchester, North Wales, Liverpool and Warrington.
No two days are the same. Today, for instance, I have changed two people's gastrostomy feeding tubes. I've trained healthcare professionals online. I've spoken to two dietitians to give them some advice and support regarding patients they were struggling and I was able to see a patient in Cumbria who has been discharged from hospital, just to make sure he was coping and managing okay.
The gentleman who’d been discharged had had all the training in hospital, he just needed a little bit more support - a bit of guidance with the feeding pump. Sometimes we’ll just be visiting to provide general care of the feeding tube, or to investigate if they suspect there might be issues. Lots of patients have wound sites where the gastrostomy tube goes in, so we need to keep a close eye on that and replace the tubes every three to four months as well - all of which is work that is carried out within patients' homes. It’s very specialised and you really get to know your patients - some of my patients have been under my care for 12 years. You become very close to them. You get to know the family, when their birthdays are and everything.
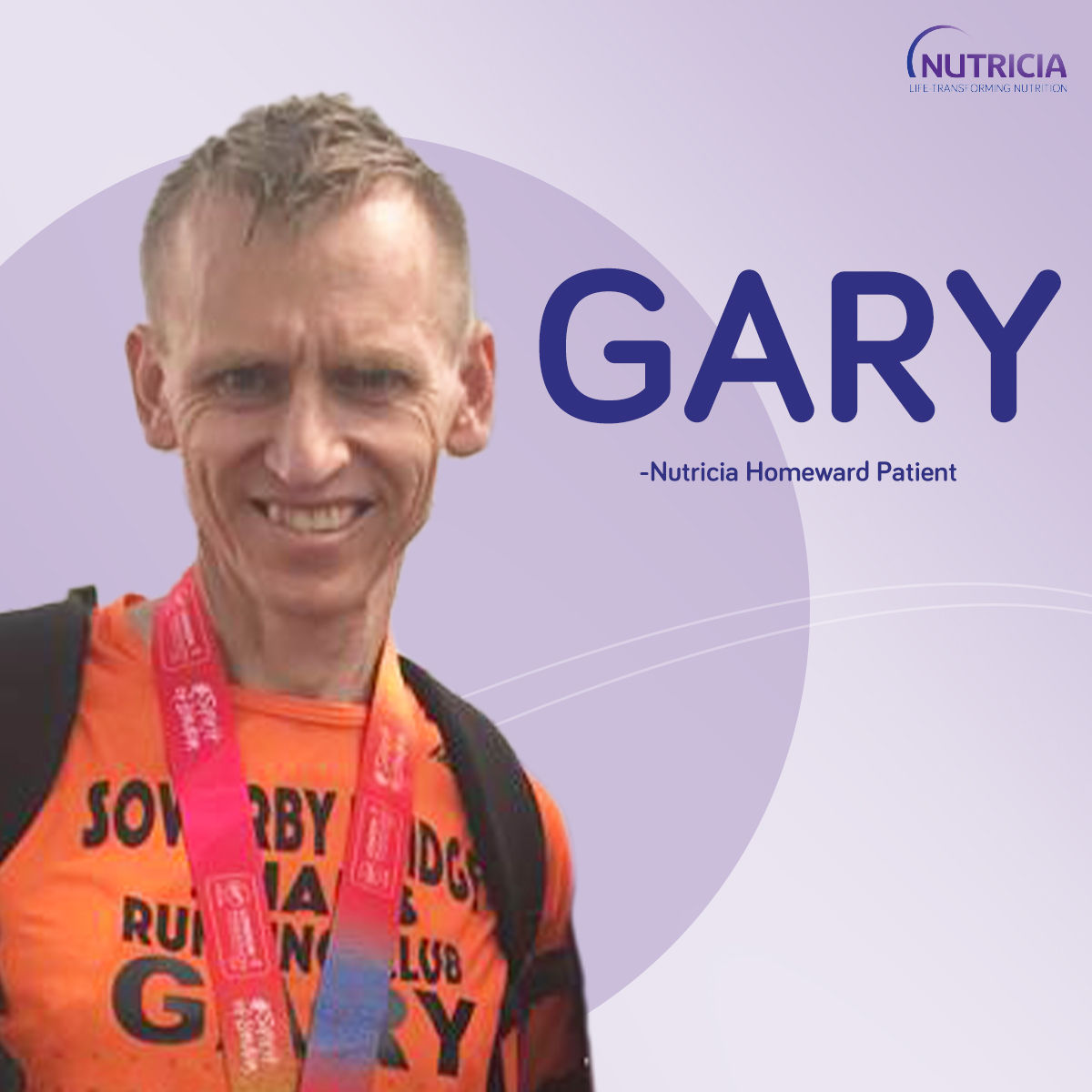
There’s another gentleman called Gary who I’m particularly fond of, and has provided several challenges for me over the last four or five years. He was quite poorly when he first came out of hospital, with a nasogastric tube which he did not like at all. He was really struggling with it, having panic attacks and ending up being readmitted into hospital. So over a period of about a month, we were able to get him a gastrostomy tube placed in his stomach, and then from that a low-profile gastrostomy feeding tube - he coped much better with that. It took quite a few weeks to get him to that stage and he was tremendously underweight. Over time he continued to struggle to maintain his weight despite taking nearly 4,000 calories a day. What we hadn't realised was that he had decided to take up running but hadn't mentioned it to anyone!
After a few months, we found out what was happening. The dietitian had called me and said “I don’t understand this - I can’t physically get any more calories into this man.” So I went out, I had a chat with him and we talked a few things through, then all of a sudden he said, “Oh, I’m training for the London Marathon!” He had a treadmill in the garage that he was pounding on day and night, so that answered a lot of questions and we were able to adjust his care appropriately.
Since then he’s done the London Marathon, and he’s been canoeing from Liverpool to Newcastle. He likes to challenge himself on a yearly basis with activities to raise money for PINNT, a charity which supports people fed by artificial nutrition. His next challenge is in June this year when he’ll be doing a run along Hardian’s Wall that is basically coast to coast. So it has been a wonderful challenge trying to keep up with him, schedule the changes of gastrostomy tube at appropriate times and support the dietitian in keeping him fit and healthy.
That’s the most rewarding part of my job: seeing my patients get better. A big part of my role is that a lot of my patients have gone through cancer treatments. So they’ve been diagnosed with throat cancer, for example, and they have a gastrostomy tube inserted prior to starting radiotherapy and chemotherapy. When that treatment is completed and they come back home, we then take care of them and eventually remove the tube when they’re better and they’ve got the all clear. That’s a nice part of my job. I enjoy that bit.
We hear so many good comments about Nutricia from all our patients. I think that’s because we have as much time to spend with them as they need - we’re not restricted to five or ten minutes when we go and see patients - and they really appreciate not being rushed and getting that support. On top of that, our products are excellent and patients really seem to like them, and I’m always hearing good things about our delivery people as well. All my patients seem really happy with Nutricia.
Just this morning, I was talking to a young girl - a granddaughter of one of the patients I was visiting - and she was telling me she wanted to be a nurse. I told her she’ll have to work hard at school, then do the three years at university, but it’s a really wonderful job to have. It will always be somebody’s dream because it’s so rewarding. You just have to go out there and get it.